|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Research Highlights |
|
We Are Living Longer than Before, But Are We Healthier?
by Prof. Jean Woo & Dr Ruby Yu Hong Kong tops the world for longevity, with residents having the longest life expectancy in the world for the third year in a row. People in Hong Kong are living longer than before, but are they healthier and ageing well? Prof. Jean Woo and Dr Ruby Yu from the CUHK Jockey Club Institute of Ageing have been trying to answer this question in their recent research. Despite significant advances in people’s life expectancy in recent years, a significant percentage of older people still require hospital services and long-term care. In 2016, older people represented only 16% of the population, but they were the main users of care services. Prof. Woo and Dr Yu pointed out that the increased use of health services by those from older age groups may be attributable not only to greater numbers of older people, but also to greater levels of frailty. Frailty is not a diagnosis, but a clinical state in which an individual is at an increased risk of developing a functional dependency or of dying when exposed to a relatively minor change in their circumstances. Why is frailty important? Older people living with frailty are likely to experience problems, to have difficulty maintaining their ability to live independently, and to be at a high risk of hospitalization due to disability and, subsequently, of institutionalization, which may lead to a poor quality of life and low levels of well-being. In 2015, Prof. Woo and Dr Yu conducted screening for frailty in the community to estimate the prevalence of frailty among older people aged 65 and older. They found that frailty is very common in Hong Kong, with a prevalence of approximately 12.5% in people older than 65 living in the community. Pre-frailty was even more common for intervention at approximately 50%, suggesting room for reversal of this state. Although frailty is common in the region, there is a lack of information about trends in frailty, physical and/or cognitive impairment, and healthy life expectancies with and without impairment. Hence, the team performed a series of analyses to shed light on these issues and provide policy guidance on plans for future elderly care services in Hong Kong. In the analysis, the team examined frailty among older people in Hong Kong and compared levels of physical and/or cognitive impairment between two elderly cohorts. The team also provided projections on the number of older people with physical and/or cognitive impairment in Hong Kong, and on the number of nurses and health care workers that would be required to care for them up to the year 2041. Meanwhile, 90,000 community-dwelling people older than 65 were studied using 12 waves of data on multiple birth cohorts from the Elderly Health Centres of the Department of Health in Hong Kong. In the analysis, the participants were classified into different cohorts according to diverse years. It was found that more recent cohorts at each age have higher levels of frailty than earlier cohorts at the same age, suggesting that older people today are experiencing higher levels of frailty in their later years than that experienced by their parents. 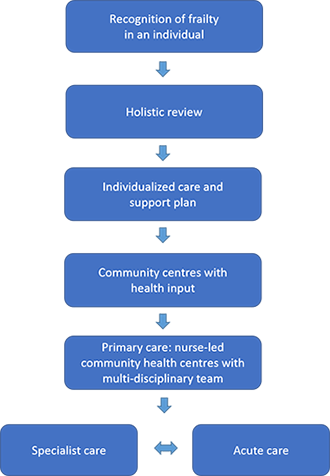 The findings on trends in frailty and physical and/or cognitive impairment imply that the gains in life expectancy are coming with increases in levels of frailty and impairment, and will lead to a greater need for medical care, social services, and long-term care services. Hence, the team proposed an algorithm for the prevention and management of frailty. The findings on trends in frailty and physical and/or cognitive impairment imply that the gains in life expectancy are coming with increases in levels of frailty and impairment, and will lead to a greater need for medical care, social services, and long-term care services. Hence, the team proposed an algorithm for the prevention and management of frailty.Frailty should be identified to improve outcomes. Interactions between an older person and health and social care professionals should include an assessment of frailty. Once a person has been identified as frail, a holistic review of medical, functional, psychological, and social needs based on a comprehensive geriatric assessment should be undertaken for care planning. The output of the holistic review should then be used to generate an individualized care plan with details of personal goals and management plans. Some individuals may be managed within the realm of primary care, some may be referred to the care of a specialist, and others may be referred to acute care. Prof. Woo and Dr Yu pointed out that the growing number of people with complex health and social care needs, particularly frail older people, means that the current health and social care system in Hong Kong is unsustainable and unable to meet current and future needs. There are three major concerns about the current state of care for frail older people. The model of acute care is unsuited to frail older people with complex needs; the time spent caring for frail older people is inversely correlated to the amount of formal training received; and providing care for older people is an endeavour that is lacking in social and professional status. To solve the dilemma, Prof. Woo and Dr Yu have been working on a community pilot project concerning a model of primary care for older people. This is the Jockey Club Community eHealth Care Project. The project began in 2016, and involves 20 community centres in all three regions of Hong Kong. An integrated medical and social model of primary care has been adopted in this community pilot project. The team aims to engage older people and NGO centres, empower older people to make effective decisions about their health, and enable the staff of the NGO centres to provide care services in partnership with the health sector. In terms of service provision and coordination, a brief geriatric assessment is provided to the participants to assess their health status and needs. Interventions are also provided, including tele-care, individualized assessments, and group-based activities that support people-centred and integrated care. An evaluation plan has also been developed to test the effectiveness and acceptability of the pilot model. Prof. Woo and Dr Yu hope that the model will be adopted as the first step in an NGO-based effort to provide primary care for older people. They also envision the project as contributing to a future in which all people have access to quality health services that meet their complex needs. ■ |